Muhammad Shamim ( Department of Surgery, Fatima Hospital and Baqai Medical University, Karachi. )
August 2010, Volume 60, Issue 8
Case Reports
Abstract
Hydatid cyst disease most commonly affects liver and lungs, but it can affect all viscera and soft tissues of the body. Simultaneous mammary and femoral hydatid cysts, without any other visceral involvement, are extremely rare. This is a case report of 25-years-old female, presenting with lump in left breast mimicking fibroadenoma and lump in right thigh mimicking fibroma. Both turned out to be hydatid cysts.
Introduction
Hydatid cyst disease results from the infestation caused by the larval stage of parasite Echinococcus granulosus. Its geographical distribution is not limited and is therefore a global health concern particularly affecting people residing in the rural areas who are in intimate contact with cattle.1 Liver and lungs are the most commonly involved organs. Rarely spleen, brain, breast, pancreas, kidney, adrenal, bladder, ovary, heart, artery, thyroid, parotid, mesentery, retroperitoneum, bone, muscle, thigh and subcutaneous tissue can be the site of disease.1-4 A case of mammary and femoral hydatid cysts incidentally found during surgery, is presented here.
Case Report
A 25 years old female presented with the complaints of lump in left breast for 3 years and lump in right thigh for 12 years. On examination, breast lump was in the upper inner quadrant, 6 x 6 cm in size, spherical, firm, non-tender and freely mobile; femoral lump was in the middle of thigh posteromedially, 2.5 x 6 cm in size, elongated, firm, non-tender and freely mobile. Breast ultrasound showed well circumscribed 5.5 x 6 x 5.8 cm area, with both echolucent as well as echogenic areas. Thigh ultrasound showed a cystic anechoic area with well defined contour, 1.8 x 1.8 x 5.3 cm. Fine Needle Aspiration Cutology (FNAC) of breast revealed eosinophilic material. Hydatid serology was not performed. On admission patient\'s hemoglobin was 8.2 gm%, and she received one unit of packed cells before operation. Excision biopsy of both lumps was planned.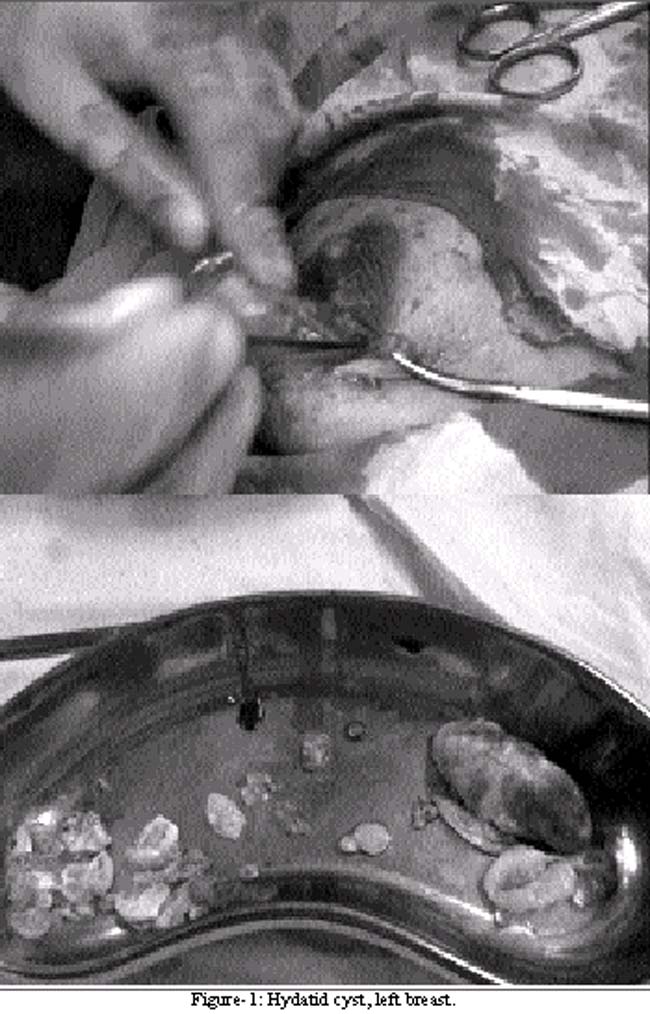
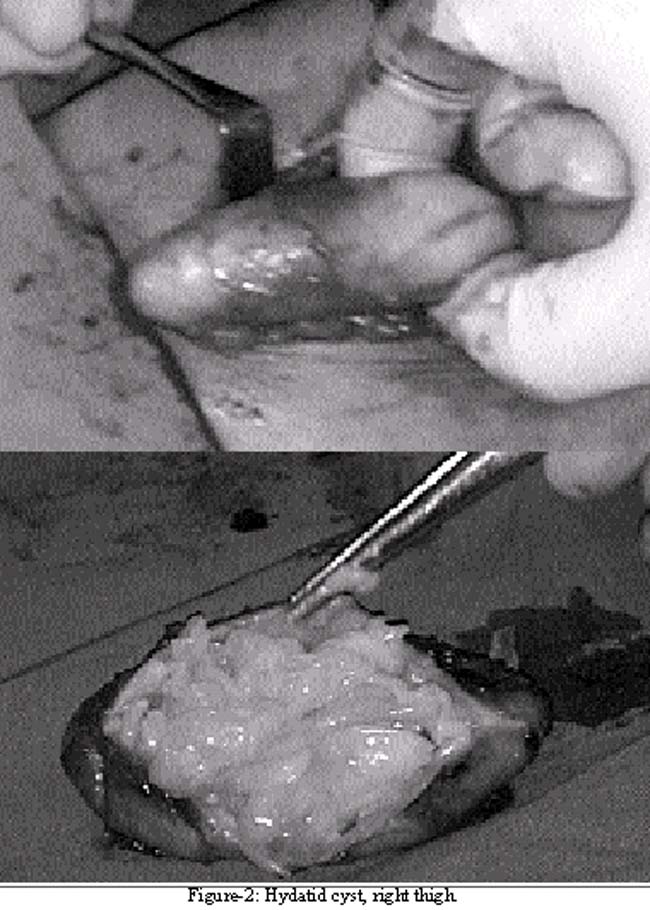
After general anaesthesia, a circumareolar incision was made in the upper inner quadrant of left breast. On attempting enucleation, adhesions of lump with breast tissue were found. During dissection, the hydatid sac was accidently opened and numerous daughter cysts were removed; there was no anaphylactic reaction. The cyst was removed in toto and wound was closed. Femoral hydatid cyst was also excised in toto; it also contained numerous daughter cysts. The post-operative period was uneventful. Histopathology confirmed hydatid cyst disease in both lumps. Abdominal ultrasound, X-ray chest, and CT scans of abdomen and chest were normal. Postoperatively patient was given a 4 weeks course of albendazole. Monthly follow-up during the first year showed gradual decline in hydatid serology. Patient was then followed annually with serology and CT scan of abdomen, chest and skull, and no recurrence was detected at the end of 3 years.
Discussion
Hydatid cyst disease may present with slowly growing mass, pain or pressure symptoms depending on the site of disease. It may involve almost any part of the body, occurring most frequently in the liver (75%), followed by the lung (15%) and the remainder of the body (10%).5,6 It may cause serious problems in the differential diagnosis when developed in unusual sites. Reported rare sites include: spleen, brain, breast, pancreas, kidney, adrenal, bladder, ovary, heart, pericardium, mediastinum, pleura, chest wall, artery, cavernous sinus, thyroid, parotid, submandibular gland, mesentery, peritoneal cavity, retroperitoneum, inguinal canal, bone, muscle, thigh and subcutaneous tissue.1-9 The breast hydatidosis accounts only for 0.27% of all occurrences.5,9 Systemic dissemination is the source of breast hydatidosis, as in this case.8 Primary site was probably the thigh (femoral) hydatid cyst, as it was present long before the mammary hydatid cyst.
In hydatid endemic areas, hydatid disease should be suspected in any patient presenting with a cystic mass, in any tissue or organ.7 The diagnosis is usually made by combination of clinical findings, imaging, and serologic tests. A high index of suspicion, peripheral eosinophilia, and a history of exposure in an endemic area gives clue to the diagnosis.8 Imaging (ultrasound or CT scan) can help in cyst localization. Mammography and breast ultrasound are non-specific, and hydatid cyst may be indistinguishable from benign cyst.4 Serologic tests, like the enzyme linked immunosorbent assay, indirect haemagglutination and immunoblot techniques gives final confirmation of the hydatid origin of cyst.8 Diagnosing breast and other superficial hydatidosis through FNAC is hazardous, as it can cause anaphylactic reaction due to fluid leakage.4 In this case the diagnosis was made per-operatively; although ultrasound and FNAC findings were suggestive when considered retrospectively, but were ignored and not properly worked up by serological tests.
Surgery is the definitive treatment of hydatid cyst disease irrespective of its location. The aims of the surgical treatment are total removal of all parasitic elements, avoidance of spillage of the cyst contents and maximum conservation of the affected viscera.8 In this case total cyst excision was made at both sites though breast cyst did rupture with spillage of the contents. Recurrence has been reported in 10% of patients undergoing hydatid cyst surgery due to spillage of protoscoleces.8 Perioperative chemotherapy using albendazole can decrease the incidence of recurrence.4 The recurrence can be detected during the follow-up by clinical and serologic evaluation. In case of rising titres, imaging is required to localize the cyst.8
Conclusion
Hydatid cyst disease should be considered in the differential diagnosis of superficial cystic lumps, and the serological tests should be performed before surgery so that appropriate prophylactic measures can be taken.
References
1.Das S, Kalyani R, Kumar U, Kumar HM. A varied presentation of hydatid cyst: a report of four cases with review of literature. Indian J Pathol Microbiol 2007; 50: 550-2.
2.Bal N, Kocer NE, Arpaci R, Ezer A, Kayaselcuk F. Uncommon locations of hydatid cyst. Saudi Med J 2008; 29: 1004-8.
3.Uysal M, Kilic D, Findikcioglu A, Tarim A, Kocer NE. Coexistence in unusual locations of hydatid cysts: thigh, breast and lung involvement. Int J Infect Dis 2007; 11: 470-2.
4.Yaqoob N, Kayani N, Shamim MS. Mammary echinococcosis: two cases and literature review. J Pak Med Assoc 2004; 54: 283-4.
5.Kiresi DA, Karabacakoglu A, Odev K, Karakose S. Uncommon locations of hydatid cysts. Acta Radiol 2003; 44: 622-36.
6.Engin G, Acunas B, Rozanes I, Acunas G. Hydatid disease with unusual localization. Eur Radiol 2000; 10: 1904-12.
7.Yildirim M, Erkan N, Vardar E. Hydatid cysts with unusual localizations: diagnostic and treatment dilemmas for surgeons. Ann Trop Med Parasitol 2006; 100: 137-42.
8.Erkan N, Haciyanli M, Yildirim M, Yilmaz C. A case report of the unusual presence of hydatid disease in the pancreas and breast. JOP 2004; 5: 368-72.
9.Abi F, Fares F, Khaiz D, Bouzidi A. [Unusual localizations of hydatid cysts. Apropos of 40 cases.] J Chir (Paris) 1989; 126: 307-12.
Journal of the Pakistan Medical Association has agreed to receive and publish manuscripts in accordance with the principles of the following committees:




