Kaukab Naeem Syed ( Department of Medicine, PIMS, Islamabad. )
August 2010, Volume 60, Issue 8
Case Reports
Abstract
Tuberous sclerosis or Tuberous Sclerosis Complex (TSC) is a genetic disorder characterized by the growth of numerous benign tumours in many parts of the body caused by mutations on either of two genes, TSC1 and TSC2. The case of a 31 year old female who fulfilled 8 major criteria of Tuberous Sclerosis Complex is reported. Multiple research work projects are being carried out on this disease, unfolding the realities regarding its etiology as well as treatment. TSC patients, besides receiving symptomatic treatment should also be offered special schooling and regular follow up by expert physician.
Introduction
Tuberous Sclerosis or Tuberous Sclerosis Complex is a genetic disorder characterized by the growth of numerous benign tumours in many parts of the body; including the brain, heart, lungs, eyes, kidneys, skin and other organs, leading to significant health problems like seizures, intellectual disability, autism or developmental delay. TSC is caused by mutations on either of two genes, TSC1 and TSC2, which encode for the proteins hamartin and tuberin respectively. These proteins act as tumour growth suppressors, agents that regulate cell proliferation and differentiation.1 The live-birth prevalence is estimated to be between 10 and 16 cases per 100,000. A 1998 study estimated total population prevalence between about 7 and 12 cases per 100 live births. TSC occurs in all races and ethnic groups, and in both genders.2 Definite TSC is diagnosed when either 2 major features (out of a total of 11) or one major feature with 2 minor features (out of a total of 9) are present.3 Tuberous sclerosis has no cure, but treatment as medicine, educational and occupational therapy can help relieve symptoms.
Case Report
A 31 year old female, resident of Islamabad, presented to the hospital through E & A department with the complaint of fits for one day. She was a diagnosed case of epilepsy since the age of one and a half months and had been on anti epileptic medication. Currently, she presented with one day history of generalized tonic-clonic fits, each lasting for one minute, with a relaxation phase observed for 5-10 minutes. She did not regain consciousness in between. The fits were associated with urinary incontinence, frothing, and uprolling of eyeballs. Tongue bite was absent as patient had no teeth. Such episodes were occurring repeatedly during the above mentioned period. There was no preceding history of fever, cough, diarrhoea or fall. Initially, in the E&A Deptt, she was given 3 bolus doses of inj. Diazepam at an interval of 15 minutes with no response. She was then started on Infusion of Sodium Valproate which controlled the seizures.
Past history was significant as she was reported to be mentally retarded. Although her milestones were not delayed, but she was only able to speak in small sentences. She experienced her first fit at the age of one and a half months. Since then, she was on carbamezapine, diazepam and chlorpromazine hydrochloride; Carbamezapine had been discontinued since last one year by her parents without medical advice. Patient had acute visual loss at the age of 13 years, which limited her social interaction and mobility. On physical examination she was found to be unconscious, lying restlessly in bed with a glasgow coma scale of 7/15. Her vitals were stable. Physical signs included pallor, facial angiofibromas (Figure-1), hypomelanotic macules (Figure-2)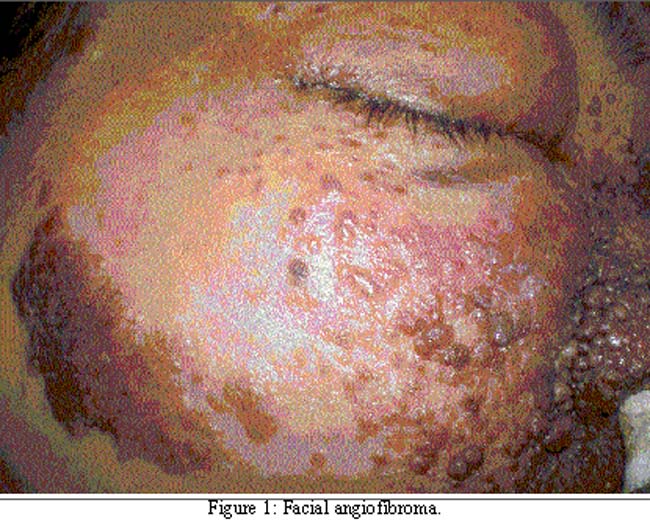
in lower abdomen, left lower limb, and epigastric region. Periungal fibromas and subungal fibrosis of left thumb were also present. A Shagreen patch was noticed in the lower right lumbar area. There was loss of denture. One rectal polyp, small in size was palpable on digital rectal examination.
Investigations showed panctoypenia with macrocytic anaemia (Hb 7.6gm/dl, WBCS 3200/cmm, platelets 21000/cmm). ESR was 47mm/1st hr. Differentiated Leukocyte Count was normal but showed 2% bands. Besides routine chemistry her serum tests included prolactin, phosphorus, and magnesium, all within normal limits. Urine routine examination was normal. In ultrasound abdomen, right kidney could not be visualized suggesting atrophic or ectopic kidney. However parenchyma of left kidney was replaced by multiple cysts and at least 2 angiolipomas. She had generalized low voltage, flat EEG not responding to hyperventilation or photic stimulation, suggestive of diffuse brain atrophy (anoxic brain damage). Chest X-ray and skull X-rays (Anterioposterior and Lateral) were normal. C.T. brain without contrast was done, which showed small nodular protrusions into the lateral ventricles with calcified foci, representing subependymal nodules, demonstrating candle dripping appearances. An area of gliosis was also seen in the left occipital horn of the lateral ventricle. Fundoscopy could not be done as patient had bilateral phthisical eyes.
Summarizing her past history, extensive physical signs and investigations, the final diagnosis of Tuberous Sclerosis Complex was made. She remained seizures free for 10 days and was ultimately discharged on levetiracetam 500mg and carbamezapine 200mg twice a day.
Discussion
Tuberous Sclerosis is an important genetic disorder that affects the patient and the family in various ways. Multiple research projects are being done around the world regarding further work up of the genes involved and treatment strategies. Now, due to an understanding of its pathogenesis, multiple drug therapies are available for certain manifestations of the disease.4 But the patient, along with symptomatic control of seizures, should also be offered special schooling, and occupational therapy. Surgery, including dermabrasion and laser treatment, may be useful for treatment of skin lesions. Multiple cases have been reported highlighting involvement of different organs in TSC. In majority, there was probable diagnosis with one major plus and one minor positive feature. In our case, however, the interesting feature was the presence of 8 major and 2 minor criteria, making it a very conspicuous presentation of TSC.
Conclusion
TSC is a lifelong condition, therefore individuals should be regularly monitored by an experienced clinician. TSC must be included in the differentials of children presenting with seizures, developmental delay, and mental retardation.
References
1.Wienecke R, Klemm E, Karparti S, Swanson NA, Green AJ, DeClue JE. Reduction of expression of tuberin, the tuberous-sclerosis-complex-gene-2 product in tuberous sclerosis complex associated connective tissue nevi and sporadic squamous and basal cell carcinomas. J Cutan Pathol 2002; 29: 287-90.
2.O\'Callaghan FJ, Shiell AW, Osborne JP, Martyn CN. Prevalence of tuberous sclerosis estimated by capture-recapture analysis. Lancet 1998; 351: 1490.
3.Roach E, Sparagana S. Diagnosis of tuberous sclerosis complex. J Child Neurol 2004; 19: 643-9.
4.Yates JR. Tuberous sclerosis. Eur J Hum Genet 2006; 14: 1065-73.
Journal of the Pakistan Medical Association has agreed to receive and publish manuscripts in accordance with the principles of the following committees:




